Airway Management
Table of contents
The primary goal of ventilation/airway management is to ensure good alveolar and tissue oxygenation
Basics
Good triple airway - head/chin tilt, jaw thurst
Bag-Valve-Mask (BVM) ventilation is a two-person skill if resources allow to achieve a good seal between mask and patient
Patient positioning
RAMPing all patients not just paediatric patients to ensure optimal position to achieve success
Lateral position is always an option, don’t discount it - if you’re putting an OPA/NPA in and not managing the airway in any other way but leaving them on their back, your doing your patient a disservice
Adjuncts
OPA and NPA are still options despite having SGA and ETT available, don’t discredit them
Tracheostomy management
Suction and vent through the tracheostomy not nose and mouth
Suction for max 10 seconds, maximum 2-3cm, maximum 3 times. If patient is conscious encourage patient to cough
Ventilations
| Age | Rate (bpm) |
|---|---|
| Newborn (up to 3hrs) | 40-60 |
| < 1 yr | 30-40 |
| 1-2 | 25-35 |
| 2-5 | 25-30 |
| 6-12 | 20-25 |
| > 12 | 15-20 |
| Adult | 10-12 |
| Asthma/COPD | 4-6 |
Newborn ventilations should be done initially with air only (not O2); premature babies blend air with 1lpm of O2
Supraglotic Airway Devices (SADs)
Primary device for advanced airway management - within current service iGel which is now available in all sizes for spectrum of patients we see
Pros/Cons
Pros
- Less risk of airway trauma and infection
- No risk of oesophegeal intubation (however doesn’t mean won’t get gastric insuflation)
- Easier and faster than placing an ETT especially with inexperienced operators
- Decreased gastric insuflation compared to BVM alone
Cons
- Non-definative against airway aspiration (though AIRWAYS2 may say otherwise)
- Can be difficult to ventilate where high airway pressures (intrinsic PEEP) - e.g. Asthma
- Reports of dislodgement when used with mCPR devices (mainly classic LMA not iGel)
- Can seal poorly (both devices if used wrong, mainly however the classic LMA)
Noting that ventilation regime should be 30:2 when using mechanical CPR device (i.e. LUCAS)
Endotracheal Intubation
When intubating, verbalise “Lips -> Teeth -> Tongue -> Epiglottis -> Velecular Space -> Lift epiglottis -> Visualise cords”
- Bougie should be used for first and really, every attempt
6 stages of intubation (6 P’s)
- Pre-oxygenate: NPA/OPA and BVM/NP/High Flow, at least 1 minute
- Preparation / Plan: Setup your equipment on right hand side of patients head, have all equipment ready and checked, ensure team aware of airway plan (e.g. “if this attempt is unsuccessful we will revert to xyz, we will do a second attempt with a different operator/better suction ready/whatever, if that fails we will escalate to a CICO event”)
- Position: Consider ramping patient with appropriate padding to achieve tragus to sternal notch positioning
- Placement: Visualising tube through cords
- Proof: See Placement confirmation below
- Post intubation care: Secure tube appropriately, circuit in place and working, post any movement reconfirm placement
Placement confirmation
- Tube has to be visualised going through the cords
- Auscultation of stomach/abdo then L and R lungs
- Rise and fall of chest
- ETCO2 reading within acceptable range (targeting 35-45mmHg with good waveform however will accept less if good waveform accepting circumstances of arrest). If less than 10mmHg or waveform really inappropriate consider likely oesophegal intubation or other failure.
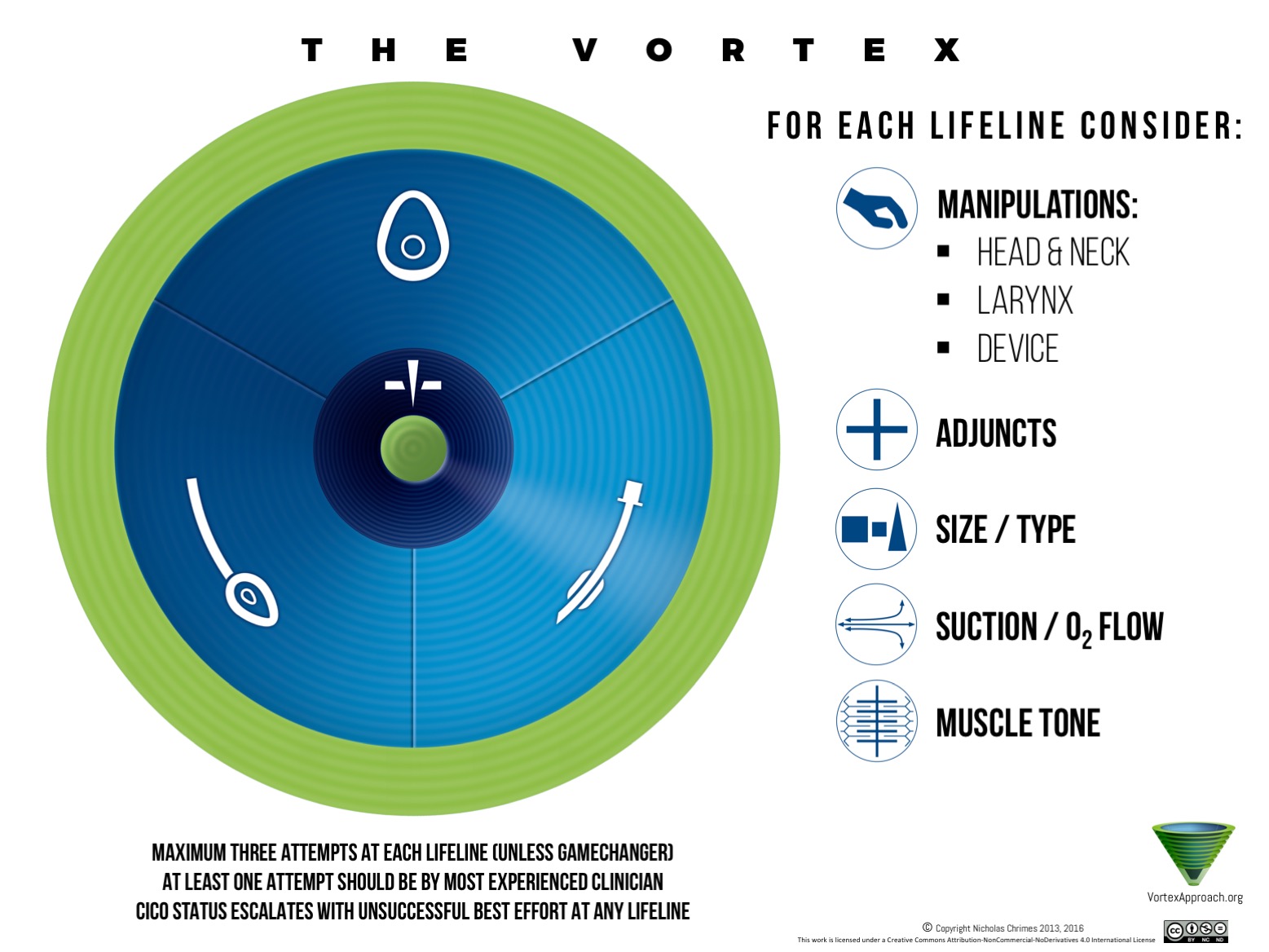
Failed intubation
Work down the Vortex ensuring appropriate troubleshooting (which includes DOPES) and if all other options have been exhausted it is imperative that you recognise a Can’t Intubate, Can’t Oxygenate situation promptly and action as required
Tips and tricks
- Can lift the entire head if required
- Rock the trachea
DOPES Check
- Displacement: ETT / iGel moved/dislodged?
- Obstruction: FBAO?
- Pneumothorax: Pneuo/haemothorax present?
- Equipment: Check from O2 cylinder to SAD/ETT and back again looking for any issues with lack of O2, lines all intact not kincked, seals all good etc.
- Secretions: Saliva, blood, vomit etc. -> Suction if yes