Asthma
Table of contents
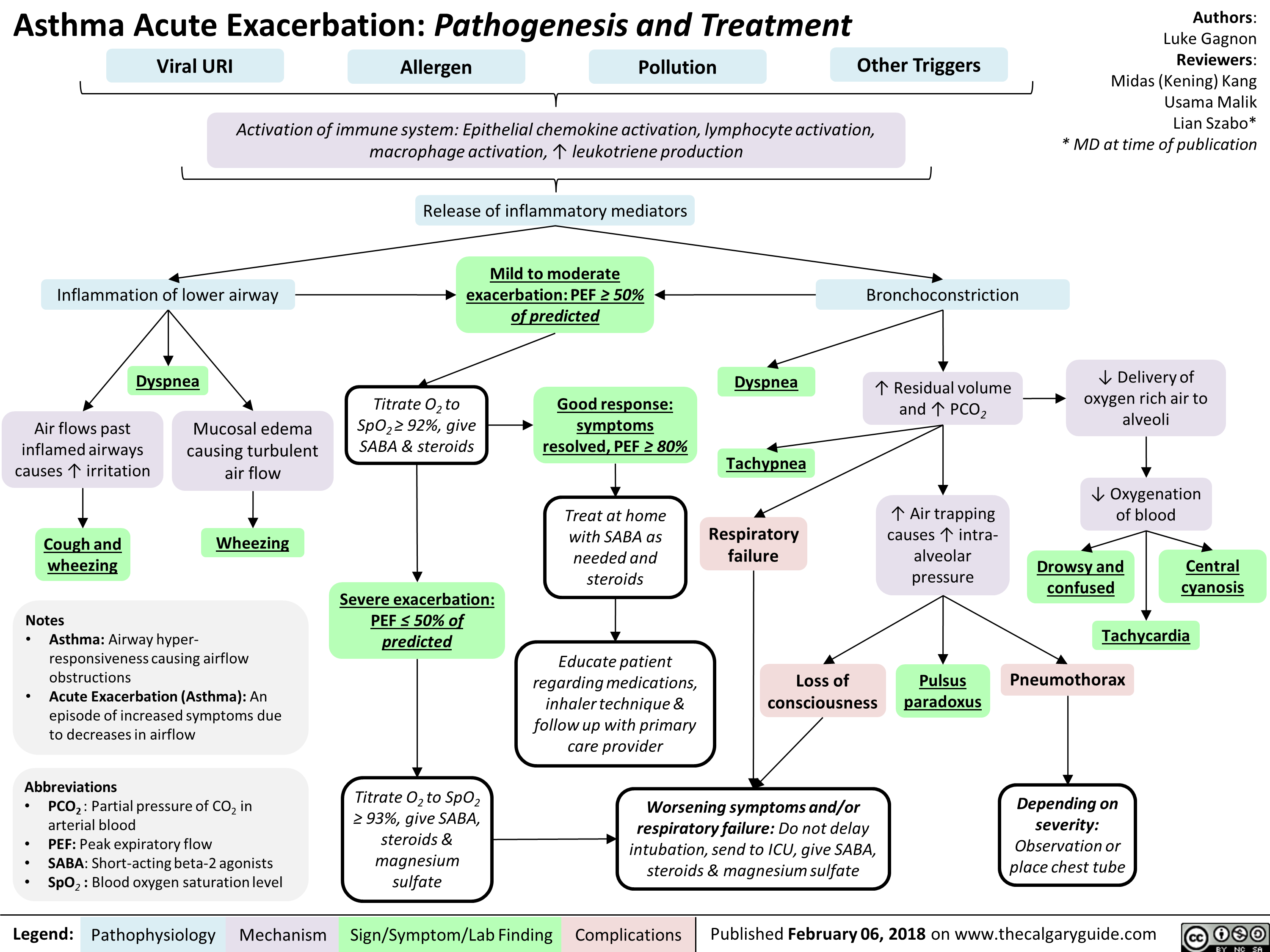
Asthma is defined as airway hyper-responsiveness causing variable and, importantly, reversible airflow obstruction.
Pathophysiology
Types of Asthma
Intrinsic
- Sometimes called non-allergic asthma
- IgE is usually only involved locally, within the airway passages
- Triggers include stress; cold or dry air; smoke; anxiety; viruses; or infections
Extrinsic
- Sometimes called allergic asthma
- Sx triggered by an allergen (e.g. dust mites, pet dander; pollen; mold)
- The immune system overreacts, produces too much IgE throughout the body (i.e. a systemic reaction). The IgE triggers the extrinsic attack.
Management
Asthma Management Plans
Patients who are engaged with a GP should have received an Asthma Action Plan which ideally uses the standard Asthma Australia format featuring actions to take “When Well”, “When Not Well” and “If Symptoms Get Worse” along with recognising an asthma emergency
A copy of a sample template can be found at on the Asthma Australia website here
Factors preventing patient compliance
Patient education
Research shows that patients often are not familiar with the correct technique for use of their preventer and reliever devices nor are they properly familiarised with their asthma action plan.
Brief interventions by ambulance staff to improve use with the patients devices, encouraging inhaler use where appropriate and referring (even informally) to see their GP again for education and an up to date asthma plan, can all be incredibly useful at decreasing repeat attendances and disease burden.
Pregnancy
Some research suggests pregnant patients are concerned about the effects of their asthma medications on their baby and as such compliance is reduced (CITE). This can lead to more frequent asthma attacks if preventer use isn’t adhered to, especially given the increased physiological stresses the mother faces during pregnancy.
Pre-hospital risk factors
When considering the presenting Asthmatic patient and the degree of clinical caution / suspicion (especially around Patient Not Transported)
- Prior ICU admission
- Prior intubation in ED
- 3 ED visits in past year
- 2 hospital admissions in last year
- 1 bronchodilator canister in last month (suggests worsening condition / increased demand)
- Chronic use of steroids
- Progressive symptoms despite best management efforts
- Patient unable to speak in sentences
Pharmocology
Types of medications used in Asthma
There are three broad groups of medications in the management of Asthma, namely: relievers; controllers; and preventers. It’s more complicated than this but for the purposes of pre-hospital understanding this is more than sufficient.
For a great poster that shows all the various Asthma / COPD medications, the National Asthma Council have produced the Asthma and COPD Medications poster (PDF).
Delivery devices
Medications for Asthma and COPD can be delivered via a range of devices - commonly seen include the pressured Meter Dose Inhaler (pMDI) which now comes with a dose counter from some brands while the other is Dry Powder Inhalers (DPI). Depending on severity, patients may have their own nebulisers (neb) but this is an ambulance/hospital level intervention for the patients we will end up called to.
Relievers
Relievers, all bronchodilators, consist of four types/groups:
- Short-acting Beta-2 agonists
- Long-acting Beta-2 agonists
- Anticholinergics; and
- Theophyllines
| Drug Class | Name | Route | Onset (min) | Uses |
|---|---|---|---|---|
| Short-acting B2 | Salbutamol | DPI, pMDI, neb, PO, IV | 5-15 | Reliever and exercise induced preventer |
| Terbutaline | DPI, SC | 5-15 | Reliever and exercise induced asthma preventer | |
| Long-acting B2 | Eformoterol | DPI | Fast, 1-3 | Reliever and controller in patients on inhaled corticosteroids |
| Anticholinergics | Ipratropium | pMDI, neb | Short | COPD and adjunct in acute severe asthma |
| Tiotropium | DPI | 30 | Long-term COPD | |
| Theophyllines | Aminophylline | Slow IV injection or infusion | Long-term COPD | |
| Theophylline | Controlled release (CR) tablets, syrup | Adjunct in severe persistent asthma |
Controllers
- Long-acting Beta-2 agonists: Examples include Indacaterol (COPD) and Salmetrolol
Preventers
- Corticosteroids: Examples include Beclomethasone, Budesonide, Ciclesonide and Fluticasone
- Cromones: Sodium Cromoglycate and Nedocromil are two examples
- Leukotriene receptor agonists: Montelukast
- Anti-IgE antibody: Omalizumab
Acute asthma management in the pre-hospital setting
Severity of asthma “attack”
| Mild/Moderate | Severe | Life Threatning |
|---|---|---|
|
|
|
Short-acting Beta-2 agonists (SABA)
Mechanism of action
Activation of β2-adrenoceptors in bronchial smooth muscle leads to increased formation of cAMP, enhancement of calcium extrusion from the cell and binding of intracellular calcium, which lowers the concentration of intracellular calcium and relaxes bronchial smooth muscle. β2-adrenoceptor agonists are the most effective bronchodilators, acting as functional antagonists of airway smooth muscle contraction.
Route
Inhaled Can be
Side effects
Beta-2 agonists stimulate cardiac stimulation which is the reason patients can present as tachycardic
IV Salbutamol
IV Magnesium
Method of action
How and why it works
Indications
When to give
Contraindications
When not to give
Cardiac Arrest in Asthma
- Low oxygen in the blood:
- May occur due to heavy mucous plugging reducing surface area for gas exchange and preventing effective oxygen uptake (Shunting)
- Hypotension
- Reduced venous return/cardiac output due to high pressures in the lungs increasing intra-thoracic pressures
- Cardiac dysrhythmias:
- Can occur as a result of the patient using excessive and/or prolonged beta agonists (ie Salbutamol).
- Commonly seen is Tachycardia (post Salbutamol and Adrenaline) rarely occasions, cause the patient to arrest
- Tension pneumothorax
- A reversible cause of cardiac arrest, common in asthmatics
- Remember that SJWA no longer endorse needle decompression in these patients
Calgary Guide