Paediatrics
Table of contents
PCH Emergency Department Guidelines
Anatomical / Physiological differences
Larger occiput (comparatively), incomplete skull fusing (hence where fontanels come from)
There is marked difference in airway anatomy which must be considered in Paediatric patients - floppier airway as hasn’t fully developed, easier therefore to occlude with positional change in either extension or flexion - must be careful with padding. Padding more likely (given larger occiput) to be under shoulders than head.
Paediatric patients have 2x the metabolic rate of adults - this means increased Oxygen requirements (and also means acidosis can become an issue far sooner)
With regards to Cardiac Output (CO), Stroke Volume in particular is fairly fixed due to developmental factors therefore there’s significantly more reliance on changing the Heart Rate component of the Cardiac Output formula hence why paediatric patients often very tachy when unwell (not just because they’re scared!)
Paediatric Assessment Triangle (PAT)
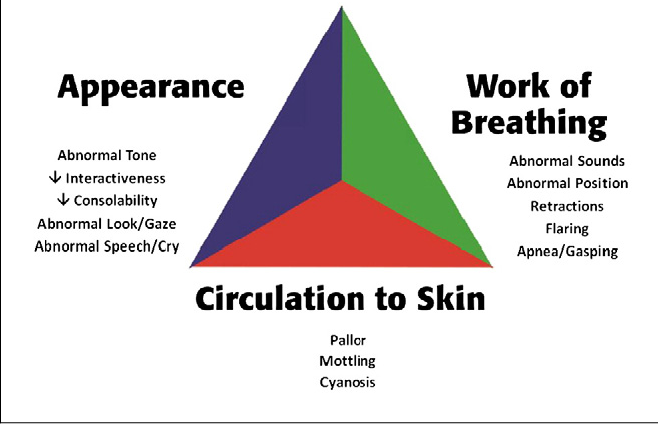
Appearance (TICLS)
- Tone
- Vigorous to limp
- Normal children of all ages, including newborns should have muscle tone
- Interactiveness
- Engaged to unintererested
- Consolability
- Content to unconsolable
- Look or gaze
- Gaze follows to glassy eyed stare
- Speech or cry
- Spontaneous speech to wimper
Breathing
- Abnormal airway sounds
- Grunting
- Stridor
- Wheezing
- Abnormal positioning
- Tripod position
- Sniffing
- Head Tilt (consider Retropharyngeal Abscess, Epiglottitis)
- Intercostal or neck retractions (or head bobbing in infants)
- Nasal Flaring
Circulation
- Pallor
- Mottling
- Cyanosis
Management priorities
- A & B: Top priorities
- C: Decompensation can happen quickly once > 30% volume lost though beware as Paeds can compensate well before falling sharply off the cliff
- D: A deeply unconcious paeds patient can have excellent recovery if cerebral hypoxia avoided (see A & B)
- E: Preserving body heat is important; make sure appropriately sized equipment is used