Diabetes
Table of contents
Diabetic Complications
| DKA | HHS | |
|---|---|---|
| Plasma Glucose (mg/dL) | >250 | >600 |
| Arterial pH | <7.3 | >7.3 |
| HCO3- (m/Eq/L) | <15mmol | >15mmol |
| Urine Ketones | Present | Minimal |
| Serum Ketones | Present | Minimal |
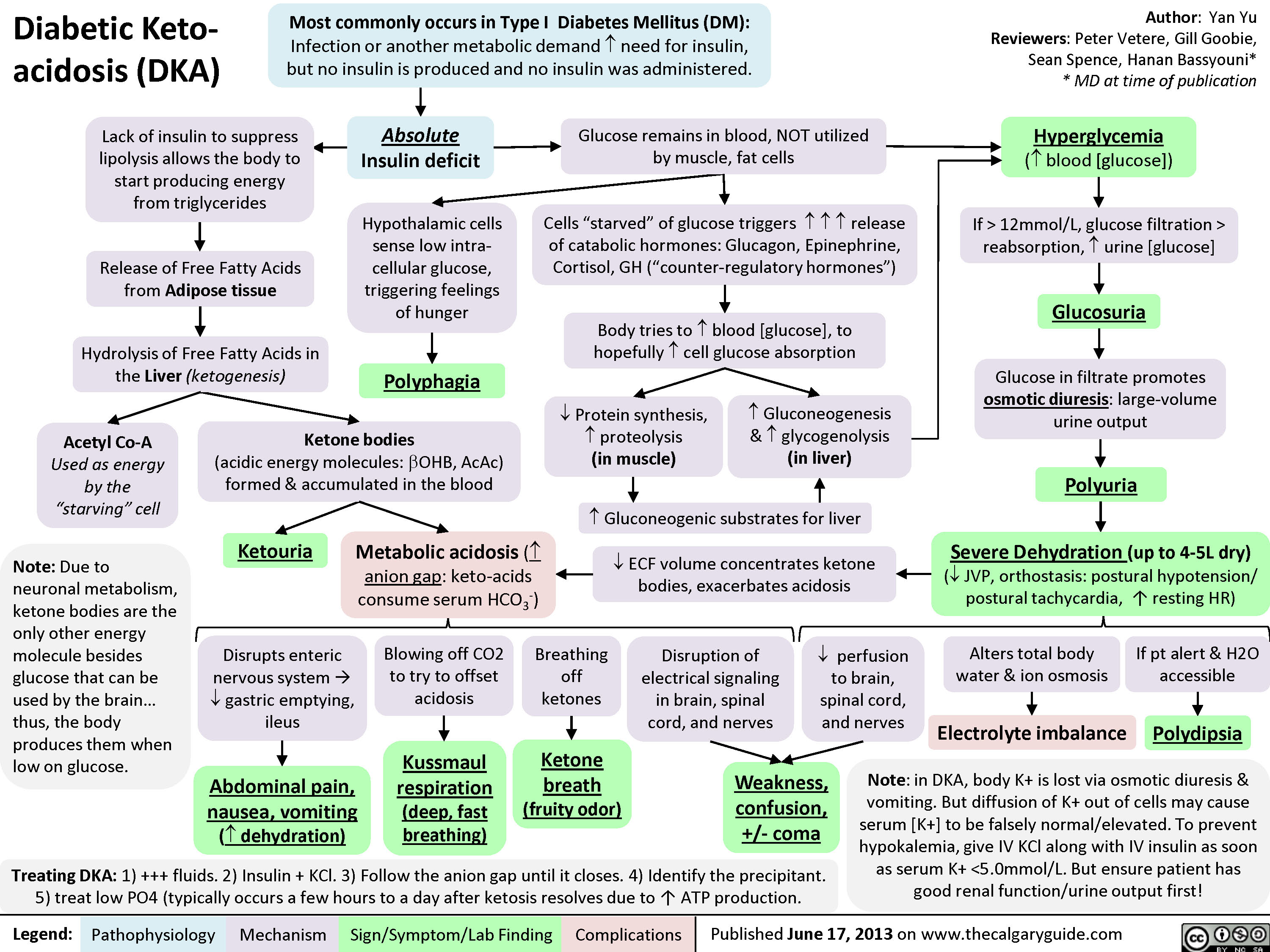
Diabetic Ketoacidiosis (DKA)
In DKA, the inability of glucose to enter cells can lead to usage of lipids as cell fuel instead of glucose. Ketone bodies are formed which are acidic.
Lack of glucose in cells can also lead to the production of cells by glycogenolysis (breakdown of glycogen into glucose) and by gluconeogenesis (creation of glucose from non-glucose stores)
- Rapid onset compared to HHS
- Absolute insulin deficiency
Causes
- Acute infection (UTI/Pneumonia)
- Myocardial Infarction
- Stroke
- Pancreatitis
Signs and Symptoms
- Hyperglycemia
- Polyuria
- Polydipsia
- Kussmaul breathing
- Acetone breath (fruity), can be a late sign, not everyone can smell it
- Dehydration
Graphical version
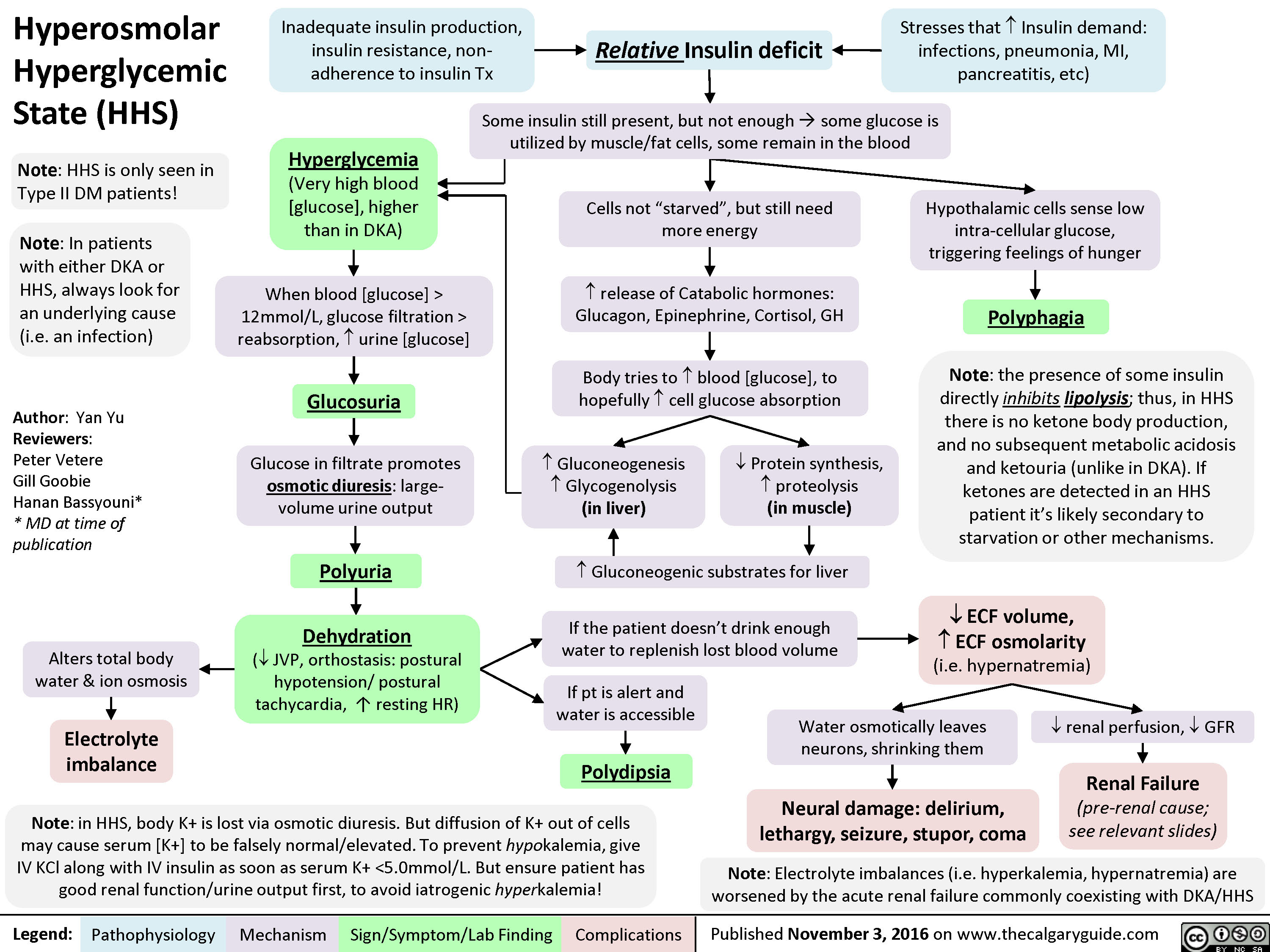
Hyperosmolar Hyperglycaemic Syndrome (HHS)
- Slower onset compared to DKA
- More common in T2DM
- Relative insulin deficency
- A deficiency of insulin to maintain normal glucose levels but enough to lipolysis (lipids are broken down) and ketogenesis (ketones are formed through breakdown of amino acids)
- Usually develops over a period of symptomatic hyperglycaemia in which fluid intake is inadequate (infection, illness) to prevent extreme dehydration due to hyperglycaemia induced osmotic diuresis.
Ketones are not present because the amounts of insulin present in most patients with type 2 are adequate to suppress ketogenesis.
- Characterised by significant hyperglycaemia, hyperosmolarity and severe dehydration (osmotic diuresis)
Causes
- Acute infections and other medical conditions
- Drugs that impair glucose tolerance (glucocorticoids) or increase fluid loss (diuretics)
- Non-adherence to diabetes treatment
Signs and Symptoms
- Severe hyperglycemia
- Altered conscious state
- Extreme dehydration
- Seizure, coma, death
Graphical version