Anaphylaxis
Table of contents
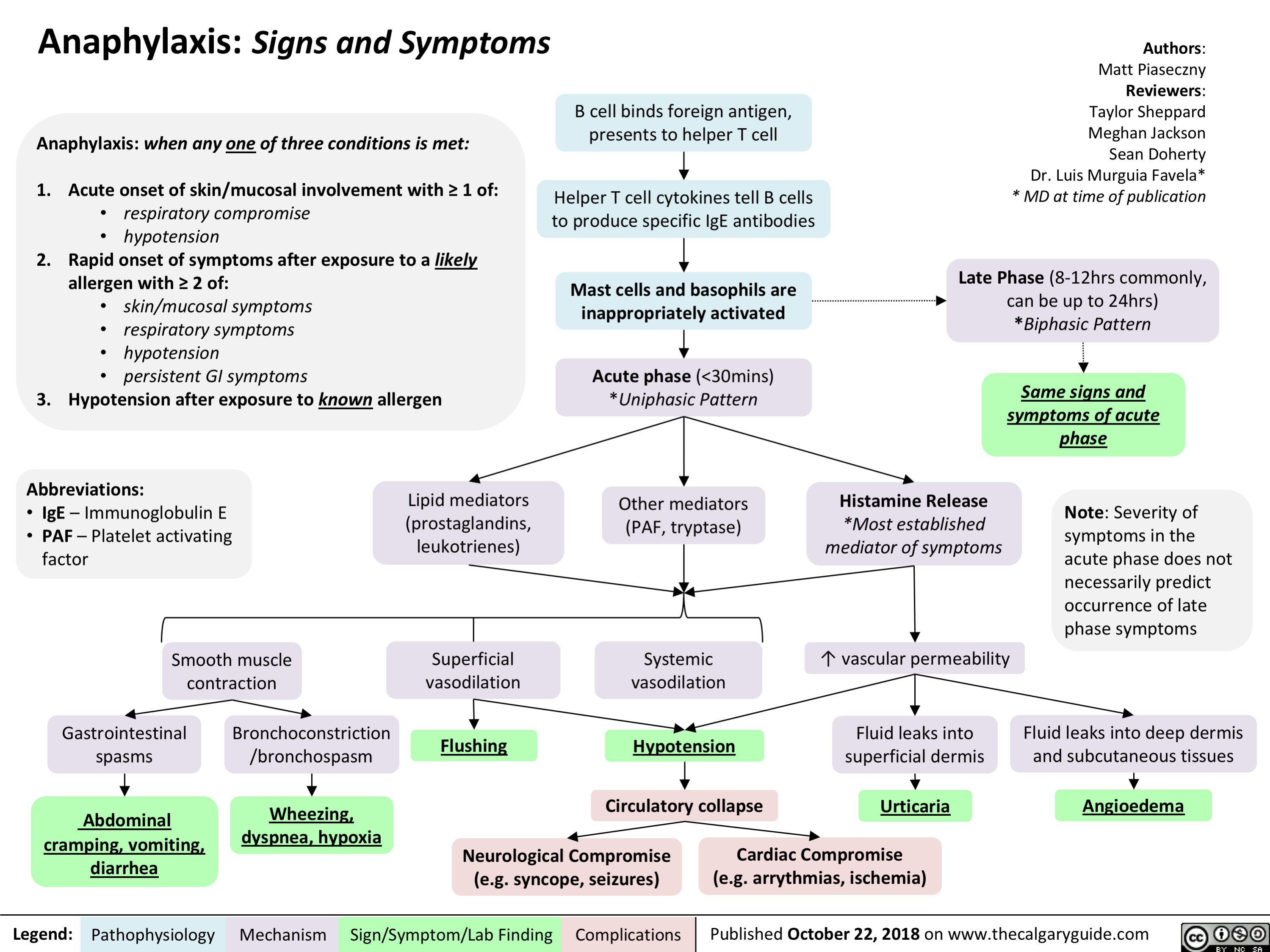
Definition of Anaphylaxis
ASCIA define Anaphylaxis as:
- Any acute onset illness with typical skin features (urticarial rash or erythema/flushing, and/or angioedema), plus involvement of respiratory and/or cardiovascular and/or persistent severe gastrointestinal symptoms; or
- Any acute onset of hypotension or bronchospasm or upper airway obstruction where anaphylaxis is considered possible, even if typical skin features are not present.
Source: https://www.allergy.org.au/hp/papers/acute-management-of-anaphylaxis-guidelines
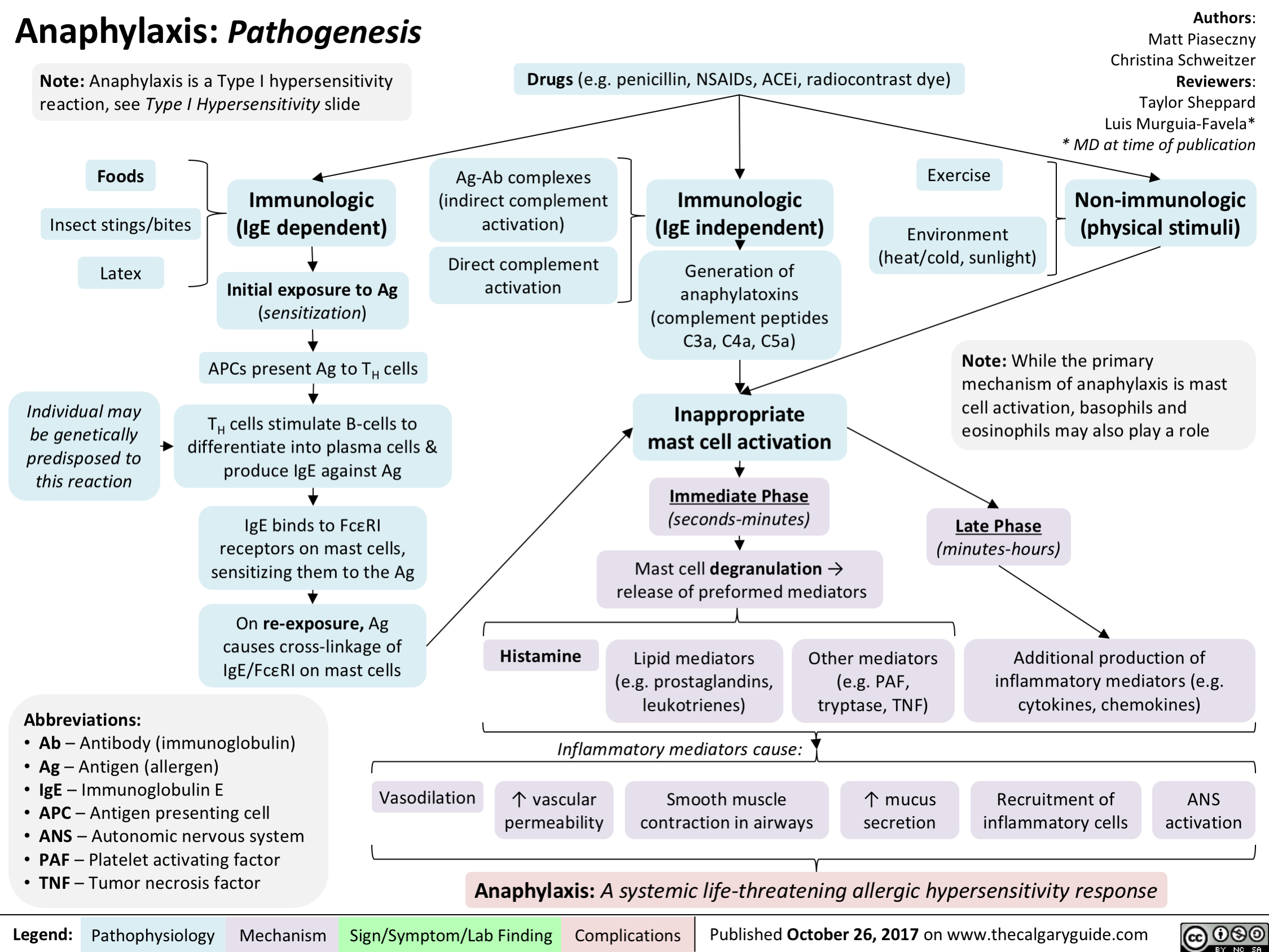
Pathophysiolgy
Primary Immune Response
Happens first time patient is exposed to the allergen
Remember:
- Mast cells: WBC present in most tissue, very prevalent around lungs, skin, nose, mouth, GI tract and other mucosal tissue
- Basophils: WBC found in blood, act in a simiar way to mast cells (i.e. they degraunlate)
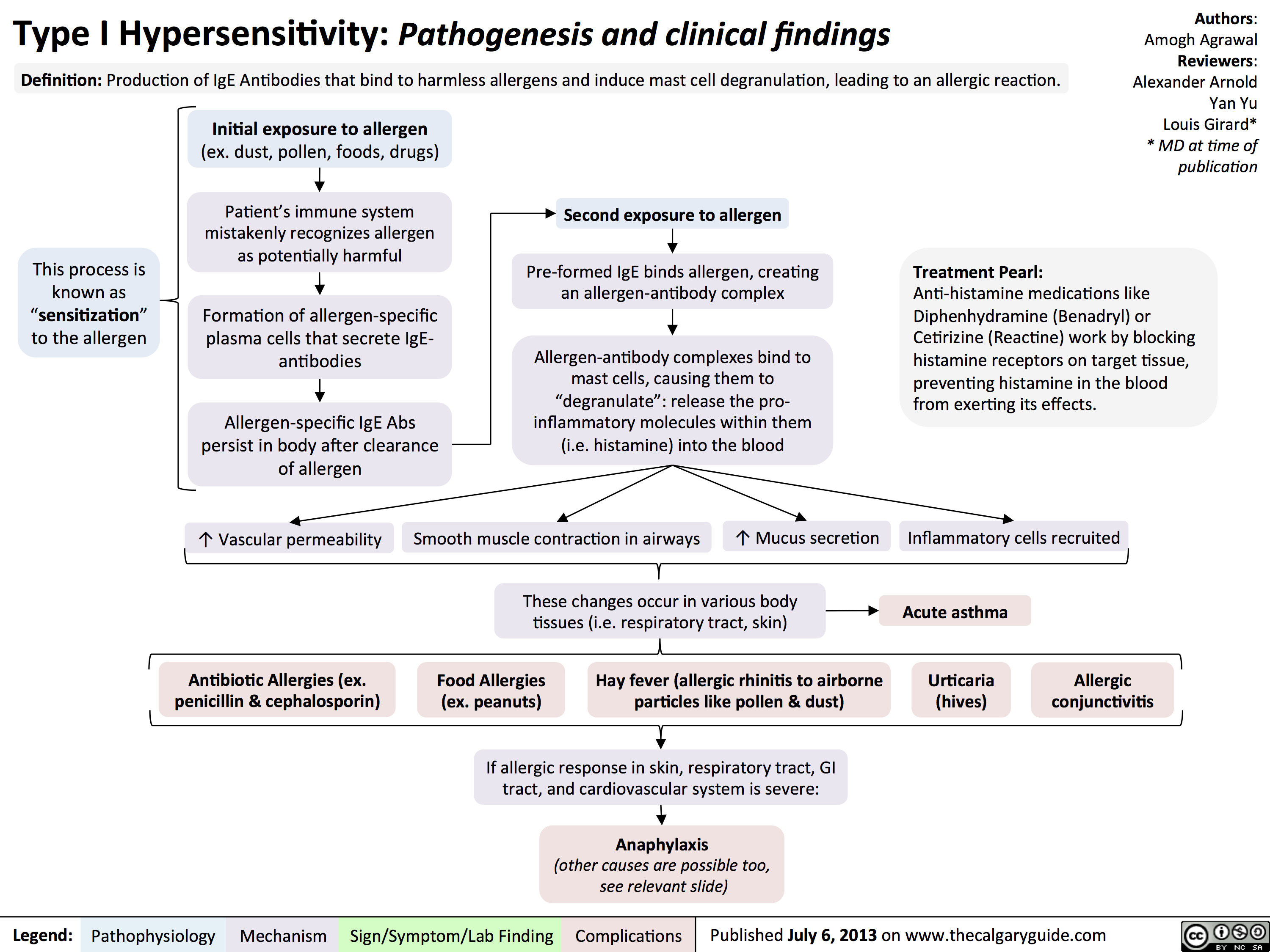
The most common type of reaction and the one we’re most interested in is the Type 1 IgE mediated reaction, the process for which goes like this:
- Antigen is either external (examples below) or internal
- Antigen enters body (if external)
- Body, in particular the immune system, triggers immune response to produce antibodies to defend against this ‘thing’
- Antigen stimulates B lymphocytes to produce antigen specific IgE antibodies
- These IgE antibodies attach to Mast Cells and Basophils and are stored
Secondary Immune Response
- Re-exposed to same allergen
- Allergen attaches to IgE antibody on the mast cell
- This attachment stimulates release of chemical mediators such as histamine from granules within mast cells (degranulation)
- Other chemical mediators including Luekotrienes, Bradykinins, Prostaglandins and Thromboxanes released
- The systemic reaction we’re familiar with occurs
Why does the systemic reacion occur?
Histamine is a vasodilator and in combination with the other chemical mediators we get massively increased vascular permiability hence the fluid shift, edema, redness etc.
Chemical mediators and what they do
Mediators
- Bradykinin:
- Cardiovascular (increased vascular permiability, vasodilation)
- Constriction of uterine and GI smooth muscle (hence the nausea and vomiting [in combo with diverted blood flow from shunting])
- Bronchoconstriction
- Histamine:
- Cardiovascular (vasodilation, increased vascular permiability, increased HR)
- Skin (irriate sensory nerves)
- Glandular secretions
- Leukotrienes:
- Bronchoconstriction
- Increased vascular permiability
- Promotes airway remoddeling
- Prostoglandin:
- Bronchoconstrictor
- Pulmonary and coronary vasoconstrictor
- Peripheral vasodilator
Effects
- Cardiovascular effects: Systemic vasodilation and increased capillary permiability -> Decreased circulating volume (as its shifted) -> Decreased BP -> Faint/dizzy
- Respiratory effects: Constriction of bronchioles and mucus production in respiratory tract -> Airway becomes obstructed -> Cough & dyspnea
- Skin effects: Histamine irritates nerve endings causing itchiness
Routes for allergen
Routes with some examples for each type
- Ingestion: Medication, nuts, shellfish
- Inhalation: Pollen, animal dander, dust, mould/mildew
- Injection: Medication, bee sting
- Skin Contact / Absorption: Latex, poisonous plants, pollen
Graphical versions
Pathogenesis
Signs and Symptoms
Type 1 Hypersensitivity